MEDICAL CLAIMS
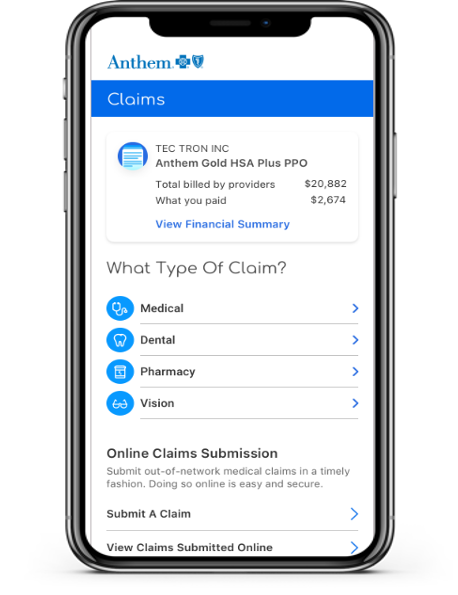
Anthem Blue Cross has two ways to process OON claims electronically: 1) via their website, and 2) via their app, available for Apple and Android devices.
If you are going to file an OON claim via the website, you log in to anthem.com. You will be presented with three options, log in (if you’re already registered), register and then log in, or use the Anthem health app, Sydney.
The registration process is simple. All that is required is the WRXA ID number from your Health Plan card, your name, and your date of birth.
Once you have registered and logged in, you then select the Claims and Payments menu item and then click on Submit a Claim. The website will walk you through all the necessary steps.
In addition, Anthem provides website help at: 866-755-2680 (M-F from 8 am to 8 pm EST) and they also have a “How Can I Help You” option available via virtual Chat.
If you want to use a dedicated app, Anthem has one; it’s called Sydney.
The site will walk you through the process.
WHY WOULD I WANT TO GO PAPERLESS?
The practical reasons are that it saves time, money, clutter, and helps the environment.
What value does this capability provide?
- Reduces OON claim reimbursement processing to an average of 2-3 weeks (as opposed to 6-8 weeks for paper transactions).
- Improves processing transparency by providing claim traceability and status.
- Provides real-time claim submission rejection notification when claim is missing required information.
- By opting to use electronic delivery of paper documents, you don’t suffer the delay of physical printing, envelope stuffing, and postal delivery. You’ll get your valuable documents more quickly.
- The PWGA spends in excess of a million dollars a year in postage and printing costs. This is money that can’t go into medical care, pension returns, or lowering premiums. By opting to go paperless, you’re helping the PWGA and helping yourself at the same time.
- For many (most) people, paper accumulates in horrifying piles of “I can’t find what I’m looking for”. Most of us throw away EOBs or other pension-related mailings and then frantically search for the data they contain come tax time. By going electronic, you guarantee that all your relevant documents are in one, easily accessible place.
- The PWGA prints approximately a million pages in a given year. A single tree produces approximately 8,339 pages of copy-grade paper after it has been stripped and pulped. By going paperless, the PWGA could save 120 trees. It’s a small amount relative to the entire country, but the next time you take a walk, count how many trees you see and then think what your walk would look like if those 120 trees weren’t there.
BLUE CROSS BLUE SHIELD GLOBAL CORE ELECTRONIC CLAIMS SUBMISSION
For outpatient and doctor care, or inpatient care not arranged through the Service Center, you may need to pay upfront. Complete a Blue Cross Blue Shield Global Core International claim form and send it with the bill(s) to the Service Center (the address is on
the form). You can also submit your claim online or through the Blue Cross Blue Shield Global Core mobile app. The claim form is available from your BCBS company or online at www.bcbsglobalcore.com.
To learn more about Blue Cross Blue Shield Global Core:
- Visit: www.bcbsglobalcore.com.
- Use the Blue Cross Blue Shield Global Core app for Android*, iPhone, and iPod touch.** (Rates from your wireless provider may apply)
- Call your BCBS company
- Call the Service Center at 1.800.810.2583 or collect at 1.804.673.1177, 24 hours a day, seven days a week
VSP ELECTRONIC CLAIMS SUBMISSION
Submitting an Out-of-Network Claim
If you’ve received eye care services from an out-of-network provider, you may need to submit a claim to request reimbursement. Your benefits will always go further when you see an in-network doctor. However, if you’d like to submit an out-of-network claim, be sure to answer all the questions and attach any receipts related to your claim.
To submit a claim request, you’ll need the following:
1. Copies of the itemized receipts or statements that include:
- Doctor name or office name
- Name of Patient (yourself or a dependent)
- Date of Service
- Each service received and the amount paid
2. Complete the claim form (this should take only a few minutes)
3. After completing the claim form, you may attach your receipt(s) OR print and mail copies of your claim form and receipt(s) to:
Vision Service Plan
Attention: Claims Services
P.O. Box 385018
Birmingham, AL 35238-5018
Tip: Missing information and receipts can delay your reimbursement. Fill out the form completely and if you’re filling it out online, snap a picture of your receipt and attach it to your claim to get your reimbursement faster. If you have receipts for other claims you must complete a separate claim form.
Don’t like filling out forms? Neither do we! That’s why we make it easy to get the most out of your benefit simply by seeing an in-network doctor. There are no claim forms to fill out when you see a VSP network doctor. Before your next visit, find a conveniently located VSP network doctor to help keep your eyes healthy and your wallet happy.
You typically have 12 months from the date of service to submit for reimbursement. Failure to submit your out-of-network claim within 12 months of the date of service may cause your claim request to be denied. Please allow up to 10 business days (plus mailing time to and from VSP) for us to process your reimbursement.
EXPRESS SCRIPTS (ESI) ELECTRONIC CLAIMS SUBMISSION
Request reimbursement:
Submit a claim if you paid full price for medicine at a pharmacy because:
- The pharmacy did not accept your member ID card by mistake
- You haven’t yet received your member ID card
- You had to buy medicine at a pharmacy outside your pharmacy network (For example, you needed to fill a new prescription while you were on a trip)
Start a Claim:
https://www.express-scripts.com/prescription-reimbursement-claim-form?partner=DCSSBOB
DELTA DENTAL
Currently, Delta Dental does not offer digital/online claim submission for out-of-network services.
ELECTRONIC EOBS
Reducing paperwork makes everything go faster as well as saving money for the Health Plan. We now offer the Explanation of Benefits (EOB) electronically so that you can quickly what has been paid on a claim and what is still owed (if anything).
How do I opt-in to receive my EOBs electronically?
- All you have to do is go to the PWGA website (www.wgaplans.org) and click on the GO PAPERLESS link you’ll find on the front page banner.
Once I Opt-In, how does it work?
- Once you elect to receive EOBs electronically, you will be notified by email every time a new EOB arrives. You can look at it online, download it to your own machine, view it on your phone, or deal with it at a more convenient time – whichever best suits your needs.
- All your EOBs are available for download via a secure portion of the PWGA website should you ever want paper copies or should you need to send them to a tax preparer or other financial advisor.
What if I try going paperless and don’t like it?
- It takes only a few clicks to opt-in for paperless delivery. It takes only a few clicks to opt-out if you don’t like it.
Is it only EOBs that are going paperless?
- We’re starting with EOBs (well over 500,000 sheets of paper a year + envelopes), but we’re going to move as much of our documentation and mailings to electronic formats as we can.
As the PWGA endeavors to bring 21st century practices into how we better service writers’ needs, we hope you will join us in our attempts to do more and to do it better.