It has become more and more difficult to get top quality surgical care in a timely manner. A new program offered by Lantern allows Writers’ Guild-Industry Health Fund participants* access to surgical procedures through their curated network of surgeons with strong outcomes – all at no cost to you. In addition to surgical providers, Lantern provides a Care Advocate to help guide you through your medical procedure, and if you need to travel to receive care, your travel expenses are also covered for you and an eligible family member, up to IRS limits.
Overview
You automatically have access to the Lantern program. As part of the program’s startup, they will send you a mailing outlining their services along with an ID card. Call Lantern to formally activate their program, which gives you the right to use their services should you desire.
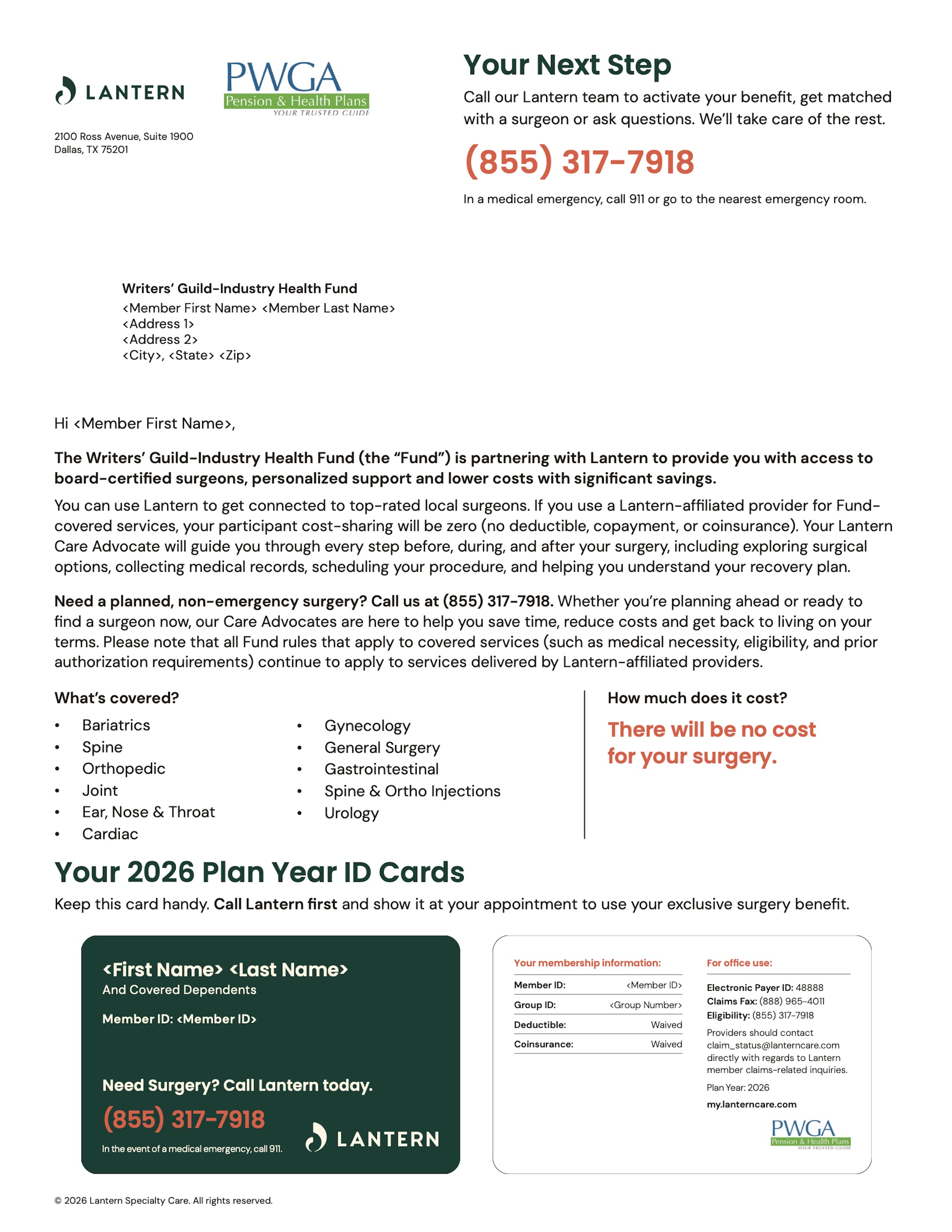
You will also receive a membership card in the mail from Lantern that looks like this:
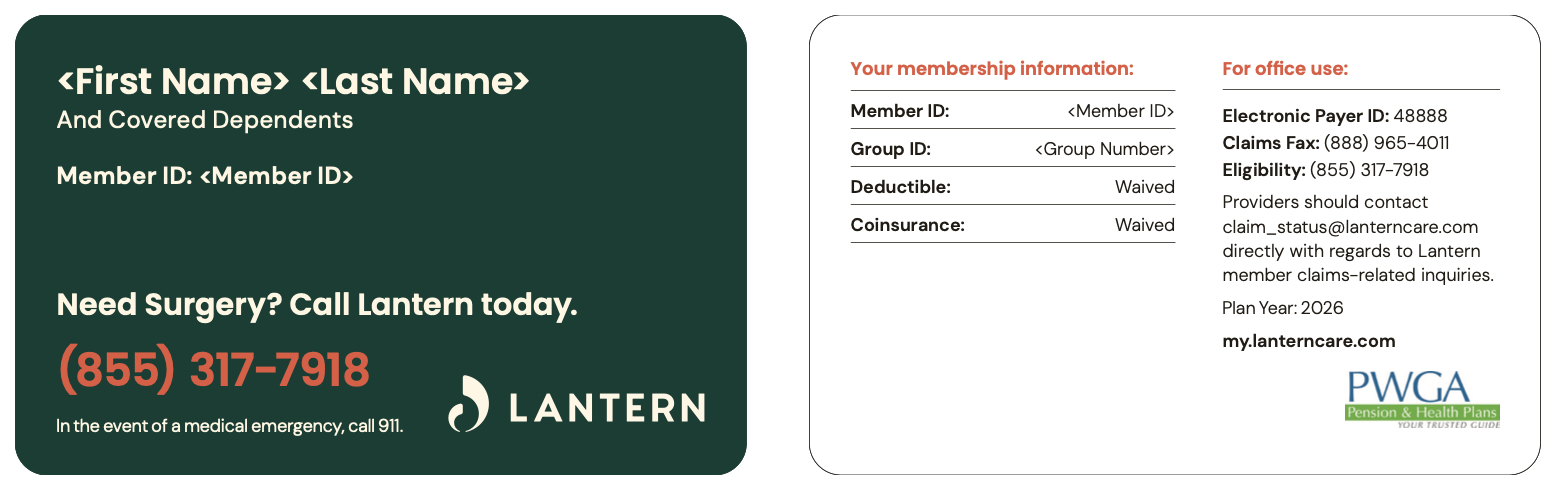
Hold on to the membership card. If you or your dependent(s) need a surgical procedure covered by Lantern, the membership card information will allow you to access Lantern’s resources.
If you elect to use the Lantern program for your medical procedure, in addition to surgeons with strong surgical outcomes, you will also be assigned a Care Advocate to help you navigate the system. Should the surgery take place in a distant city, travel, lodging, and meal expenses will be covered for you and an eligible family member, up to IRS limits.
The Lantern program is optional, so you can elect to use your current Health Plan benefits and protocol if you decide that is a better course of action. Lantern is a new resource, but does not replace your ability to choose a different care provider.
How It Works
If you have a procedure coming up, starting January 1, 2026, you will be able to contact Lantern before scheduling care. You will be assigned a Care Advocate at that time who will learn about your needs and explain your options.
The Care Advocate will help you:
- Find the right surgeon
- Coordinate appointments
- Handle paperwork
- Understand your treatment and recovery plan
- Assist you in making travel arrangements if needed
If your surgical procedure requires travel, your associated expenses will be covered for both you and an eligible family member, up to IRS limits.
The Care Advocate will be your go-to resource both before and after surgery. Before the surgery, they will let you know what is covered and part of their program, and handle reimbursement for all covered expenses. Lantern will also assist with post-surgical recovery. All of this at no cost to you.*
What is Covered and What is Not Covered
Emergency surgeries, cosmetic procedures, and some medical equipment are not covered. Your Care Advocate will explain all your options and considerations.
If you already have a surgeon, you can use them if they are in the Lantern network, but you have to contact Lantern before you have your procedure to ensure savings.
If the surgeon is not in the Lantern network, then the procedure will not be covered under the Lantern program. Coverage of services using a non-Lantern affiliated surgeon will be subject to the terms of the Writers’ Guild-Industry Health Fund.
Covered services include the following procedures:
- Joint Replacement
- Spine
- Bariatric
- Orthopedic
- Gynecology
- Cardiac
- Ear, Nose, & Throat
- Gastroenterology
- Spine & Orthopedic Injections
- General Surgery
- Urology
*Lantern is not available to plan participants who have Medicare as their primary coverage.
Summary
If you plan to have a surgical procedure, call Lantern and learn what resources are available to you. They will assist you in identifying the best surgeon for your procedure and make sure all your clerical, informational, and economic needs are addressed.
You will be receiving more information directly from Lantern upon program launch (January 1, 2026), after which Lantern will be your primary source of contact for these services rather than the Fund. However, should you have any general questions or concerns before – or after – January 1, you can contact the PWGA’s Participant Services: (818) 846-1015 or (800) 227-7863 (follow the menu prompts).